Colposcopy
Dr. Nelson Soucasaux, Brazilian gynecologist
Developed by Hinselman in Germany for helping in the early detection
of cervical cancer (and always used in conjunction with the current cytological
- cell - examinations), the colposcope is an optical device that allows
the observation of the uterine cervix (as well as vagina and vulva) with
a magnification of about 10X to 15X. Through the colposcope we can easily
visualize small details of the tissues of the uterine cervix in their normal
and abnormal aspects, typical and atypical, benign, pre-malignant and malignant.
 |
 |
| The colposcope, right, at the business end of an examination table. |
The colposcope ready to use. |
Though in clinical practice the current cytological examinations
(the "Pap tests" or "Pap smears") are much more
important than colposcopy for the early detection of all cervical cellular
atypias (and therefore for the early diagnosis of cervical cancer),
colposcopy is also fundamental for any correct clinical examination of
the uterine cervix. Here we must emphasize that there are also several
usually slight cervical epithelial atypias with normal cytological results
that can only be detected through colposcopy. Despite the importance of
the normal cytological results, cases like these may require more attention,
as, for instance, cervical cytological examinations carried out more often,
with smaller intervals. We also cannot forget the existence of false-negative
results in some cytological examinations.
Sometimes we can rule out a false-negative cytological result simply
through the colposcopic observation of areas of accentuated atypical epithelium
on the cervix. Colposcopy is also essential for the clinical evaluation
and correct management of the usual inflammatory processes of the uterine
cervix, of the very frequent "eversions" of the endocervical mucosa
and their process of resurfacing at the ectocervical epithelium, as well
as for the detection of small lesions caused by the HPV (human papillomavirus).
Whenever a cervical biopsy has to be performed, colposcopy is fundamental
for guiding the procedure to the areas of the uterine cervix that visually
exhibit more accentuated epithelial abnormalities. It is important to emphasize
that all cervical biopsies that are not performed under a careful colposcopic
control can be considered as "blindly-performed biopsies" and,
therefore, as not reliable.
Before continuing, let us briefly introduce some basic concepts on cervical
pathology. As I observed in my article "The Uterine
Cervix," published here at the MUM, in the uterine cervix there
is a strange focus of epithelial "unquietness" related to a physiological
process by which the usual eversions of the endocervical mucosa are resurfaced
by the squamous stratified epithelium typical of the ectocervix, giving
rise to the so-called "transformation zones." A collection of
irritative, inflammatory and infectious factors collaborate for making the
area of these eversions the site of sometimes problematic histological changes.
The main infectious factor responsible for the development of cervical epithelial
atypias is the HPV (human papillomavirus).
Fortunately, in most cases this epithelial "unquietness" is
benign, and the new squamous stratified epithelium that develops for resurfacing
the ectopic area of glandular epithelium is entirely normal. In such cases,
the result is the formation of what we call a "typical transformation
zone." However, with some frequency this cellular proliferation gives
rise to several degrees of epithelial atypias and abnormalities, resulting
in the development of "atypical transformation zones." Among the
abnormalities that may develop there are, in increasing order of severity,
the slight, moderate and accentuated "cervical dysplasias" and
the carcinoma in situ of the cervix. The carcinoma in situ
of the cervix is the initial stage of cervical cancer, while it is still
restricted to the epithelium. At this stage it is non-invasive and can be
easily and successfully treated through very small surgical procedures.
The formerly known "cervical dysplasias" are presently named "cervical
intraepithelial neoplasias" ("CIN") or "squamous intraepithelial
lesions" ("SIL").
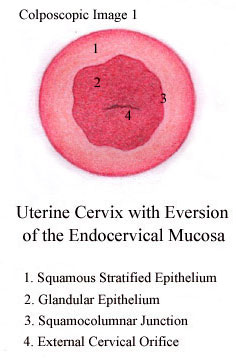
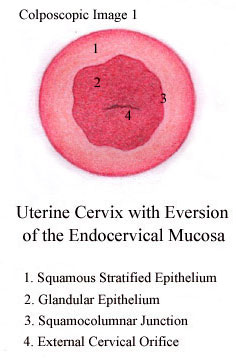
As to the aforementioned eversions of the endocervical mucosa, they
appear as reddish areas surrounding the external cervical orifice, in sharp
contrast with the clear pink colour of the ectocervical and vaginal mucosa.
The reddish aspect is simply the normal colour of the glandular mucosa,
covered by a single-layered columnar epithelium. On the other hand, the
clear pink colour is that of the squamous stratified epithelium that covers
the ectocervix and the vagina. The enormous differences between the two
kinds of epithelium that surface the uterine cervix are clearly seen at
the colposcopic examination. While the glandular epithelium exhibits a reddish
irregular surface that looks like a multitude of very small "bunches
of grapes," the squamous stratified epithelium exhibits an entirely
smooth clear pink surface.
Eversions of the endocervical mucosa are very frequent mostly in young
women and, in the absence of inflammation and other alterations, are considered
as normal and physiological. The ectopic glandular epithelium that characterizes
these endocervical eversions usually is gradually replaced by the squamous
stratified epithelium typical of the ectocervix, and the several stages
of this physiological process can be easily observed through the colposcope.
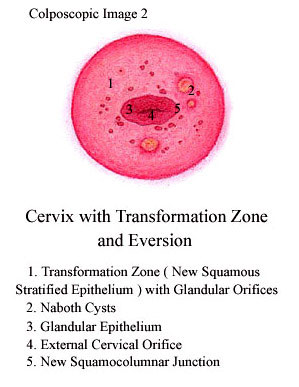
As already mentioned, the result of the replacement of the ectopic glandular
epithelium by the squamous stratified one is the development of an area
known as "transformation zone." A typical transformation zone
can be easily recognized at the colposcopic examination as an area of squamous
stratified epithelium usually containing remnants of glandular epithelium
that appear as small glandular openings and the so-called Naboth cysts.
 |
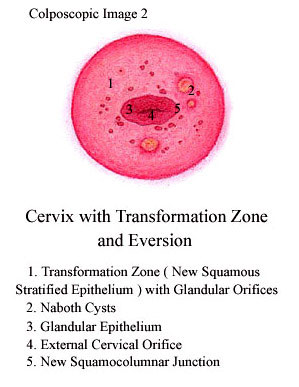 |
| This is what your doctor sees through his colposcope - although only
the most organized woman would have numbers in place. |
|
Nevertheless, the physiological process through which the transformation
zones are formed frequently gives rise to several kinds of epithelial atypias,
resulting in "atypical transformation zones". Some of these epithelial
atypias may give rise to cervical cancer, therefore the importance of their
early recognition. Even so we must remark that, fortunately, most of
them do not evolve to cancer, and this fact must be strongly emphasized
for not scaring women unnecessarily. The fundamental thing here is permanent
control through the periodic preventive examinations.
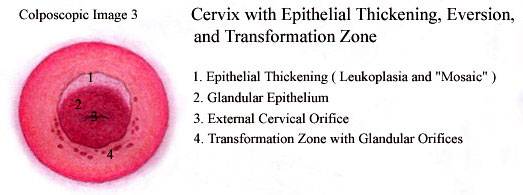
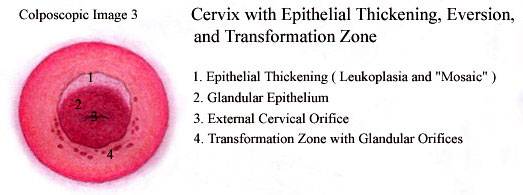
Besides the obvious aspect of carcinomatous tissue, the most important
atypias of the uterine cervix easily observed at colposcopy are epithelial
thickenings and abnormal blood vessels. The colposcopic aspects described
as "epithelial thickenings" include several alterations such as
leukoplasias, "mosaics" and "white epithelium," and
we must observe that they are very frequent. Nevertheless, these alterations
usually only require a biopsy in the presence of important cytological abnormalities
and/or accentuated degrees of thickness verified at colposcopy (as well
as atypical blood vessels ). Here we must remark that the simple presence
of areas of slight epithelial thickenings in the uterine cervix is a very
common colposcopic finding and, in such cases, the results of repeated cytological
examinations are almost always normal.
Before finishing this very brief introductory article on colposcopy,
we must emphasize that, despite the enormous importance of this procedure
on the study of the uterine cervix, the definitive and correct diagnosis
of any important cervical pathology only can be obtained through cytological
and histo-pathological examinations. This means that colposcopy alone cannot
precisely establish the correct diagnosis of any cervical epithelial atypia,
as well as any other important cervical lesion, and this must be very clear.
Copyright 2003 Nelson Soucasaux (text, illustrations and photographs
)
__________________________________________
Nelson Soucasaux is a gynecologist dedicated to clinical, preventive
and psychosomatic gynecology. Graduated in 1974 by Faculdade de Medicina
da Universidade Federal do Rio de Janeiro, Brazil, he is the author of several
articles published in medical journals and of the books "Novas Perspectivas
em Ginecologia" ("New Perspectives in Gynecology") and "Os
Órgãos Sexuais Femininos: Forma, Função, Símbolo
e Arquétipo" ("The Female Sexual Organs: Shape, Function,
Symbol and Archetype"), published by Imago Editora, Rio de Janeiro,
1990, 1993.
Web site (Portuguese-English): www.nelsonginecologia.med.br
<http://www.nelsonginecologia.med.br>
Email: nelsons@nelsonginecologia.med.br